THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.
An experimental eye cancer drug reverses memory problems in a mouse model of fragile X syndrome, according to a new study1.
The drug targets a protein that the study newly identified as being important in fragile X syndrome. If it shows promise in people with the syndrome, it could also be repurposed as a therapy for autism.
Scientists have tested numerous drugs for fragile X syndrome, the most common form of inherited intellectual disability in people and a single-gene cause of autism. Many of these drugs have shown positive results in mice, but at least 10 have failed in clinical trials.
The cancer drug, called nutlin-3, hits a novel target: a protein that is too abundant in fragile X syndrome and hinders the maturation of neurons. Whereas other experimental fragile X treatments have altered neuronal signaling, this one boosts the number of mature neurons.

Elizabeth Berry-Kravis explains how new ways to test fragile X treatments in mice may solve problems with behavioral measures. Read more.
“We discovered a novel mechanism underlying fragile X syndrome, and we provide another way to look at the therapeutic possibility for this disease,” says lead researcher Xinyu Zhao, professor of neuroscience at the University of Wisconsin-Madison. The study appeared in April in Science Translational Medicine.
The new finding adds significantly to our understanding of fragile X syndrome, says Randi Hagerman, medical director of the MIND Institute at the University of California, Davis, who was not involved in the study.
“There are many things to be excited about here,” Hagerman says. “They’ve described a new mechanism that causes dysregulation. [And] they’ve found a very specific treatment that can rectify this dysfunction.”
Cell booster:
Fragile X syndrome results from absence of the protein FMRP. People with the syndrome have difficulty with language, communication and eye contact. Mice that lack FMRP are not perfect models of fragile X because they lack many of the issues seen in people with the condition.
But fragile X mice have trouble with object recognition and spatial memory — for example, they have difficulty finding familiar objects that have been moved. Both skills depend on the hippocampus, a brain center for learning and memory.
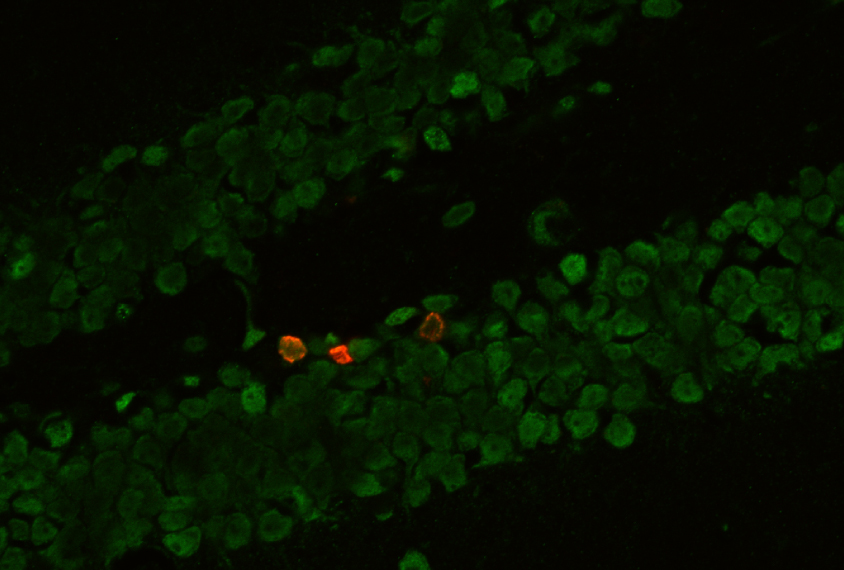
The mutant mice show a lack of neurons in the hippocampus because the available neural stem cells fail to mature.
To find the cause of this shortage, the researchers scoured a list of 417 genes that FMRP regulates. They turned up one, MDM2, which is known to be involved in the maturation of neural stem cells.
The absence of FMRP releases a brake on MDM2 expression, causing the protein to accumulate in the mutant mice, the researchers found. The excess MDM2 leads to accelerated destruction of a protein called p53, resulting in too few mature neurons.
When the researchers used chemical tricks to lower MDM2 expression in the mice, the number of mature neurons rose. They then looked for a drug that might inhibit MDM2 and found nutlin-3, a small molecule in early-stage clinical trials for eye cancer.
The researchers injected nutlin-3 into the mutant mice every other day for nine days. When they then looked in the hippocampus of the mice, they found that the number of mature neurons had risen to typical levels.
Tricky work:
The treated mice also show improvements in object recognition and spatial memory. When a researcher placed a new object in the mice’s cage, the animals no longer ignored it, but spent time actively sniffing it, as typical mice do. And after a scientist moved an object to a new location in the cage, the treated mice quickly found the object.
Some researchers caution, however, that the study is unlikely to lead to a therapy for fragile X — or autism — any time soon. “The long-term effects of nutlin-3 have not been well characterized,” says Maija Castrén, a neurologist at the University of Helsinki in Finland, who was not involved in the study.
Determining the effectiveness of nutlin-3 for autism or fragile X syndrome is likely to be tricky, too, Zhao says. The absence of tumor cells shows that a cancer treatment works, he says. By contrast, far more subjective measures, such as questionnaires and clinical exams, are the arbiters of a therapy for a neurological condition.
The history of disappointments in fragile X drug development provides a grim backdrop for any drug candidate.
“Clinical trials for fragile X have shown that treating the human condition is significantly more difficult than rescuing a phenotype in animal models,” says Michael Tranfaglia, medical director and chief scientific officer of the FRAXA Research Foundation, who was not involved in the study. “These previous disappointments only highlight the need for more therapeutic options.”
By joining the discussion, you agree to our privacy policy.