THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.
Mice with the mutations linked to tuberous sclerosis make too little protein in their brains, according to a new study1. The finding contradicts the idea that the mutations stimulate protein synthesis — a leading theory about the condition — and may have implications for its treatment.
Tuberous sclerosis is caused by mutations in either TSC1 or TSC2 and is characterized by benign tumors throughout the brain and body. Roughly half of all children with the condition have autism.
Mutations in either gene are known to decrease levels of the corresponding protein and boost activity in a signaling pathway called mTOR. This pathway increases the expression of several proteins involved in protein synthesis, so boosting its activity is thought to rev up the overall production of proteins in the brain.
The new study upends that hypothesis.
“It’s so unexpected,” says lead researcher Carolyn Beebe Smith, senior investigator at the U.S. National Institute of Mental Health. “Initially, I looked at it in this very simplistic way: If you have less TSC [protein], you’ll activate mTOR, and therefore you’ll have increased rates of protein synthesis. Obviously, nature is much more complicated than that.”
In 2011, another team showed that mice missing one copy of TSC2 show dampened protein synthesis in one brain region2. In the new work, Smith and her colleagues tracked protein levels across more than a dozen brain regions in the mice.
Their findings are surprising because a number of other studies support the expected increase in protein synthesis in the brain, says Peter Tsai, assistant professor of neurology and neurotherapeutics at the University of Texas Southwestern Medical Center in Dallas, who was not involved in the study.
Those studies tracked protein synthesis in a variety of TSC mouse models, including mice lacking one or both copies of TSC1 or TSC23. By contrast, the 2011 study and the new study both relied on a mouse model that lacks one copy of TSC2.
“If it’s true, it’s a game-changer; we would have to think really hard about the dogma,” says Tsai. But “there are still some questions I would want answers to before I wholesale buy in,” he says.
Bulk measurement:
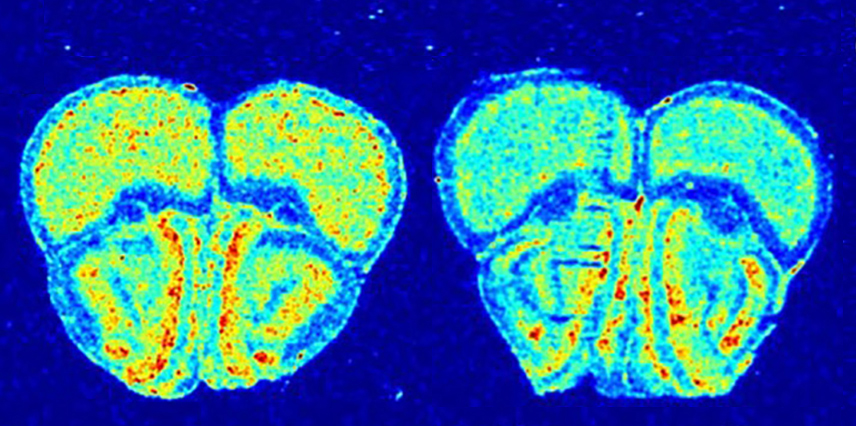
Smith and her team infused mice with a radioactive version of the amino acid leucine. After an hour, they charted radioactive fluorescence in 17 brain regions to measure levels of new protein.
Protein synthesis is dampened in all but one of the brain regions in the mutant mice, they found. Affected regions include the cerebral cortex, the amygdala and the hippocampus. The findings appeared 24 January in the Journal of Neurochemistry.
However, an overall measure of protein synthesis does not reveal what happens in particular molecular pathways or subsets of proteins.
“I suppose it boils down to this: What exactly are you measuring when you do a bulk measurement of protein synthesis? I think the answer is more complicated than you might assume at first blush,” says Mark Bear, professor of neuroscience at the Picower Institute for Learning and Memory at the Massachusetts Institute of Technology. Bear was not involved in the new study but led the 2011 work.
That study suggested that boosting the mTOR pathway increases the production of some proteins, which in turn lower the overall production of proteins. His team has also shown that in fragile X syndrome, another condition linked to autism, there is an overall increase in this larger group of proteins.
Together, the studies suggest that fragile X syndrome and tuberous sclerosis arise from opposing molecular mechanisms. Consistent with this idea, a study published in January showed that rapamycin, an mTOR inhibitor in clinical trials for tuberous sclerosis, worsens features in fragile X mice.
Smith’s team plans to give rapamycin to mice lacking one copy of TSC2 to see whether the drug boosts protein synthesis.
Target practice:
Another new study, published in February, connects the pathways that underlie tuberous sclerosis and fragile X.
In that work, researchers coaxed skin cells taken from individuals who lack one copy of TSC2 into neurons4. All of the neurons show increased expression of genes in the mTOR pathway, and some of them show a decrease in FMRP, the protein missing in fragile X syndrome. The findings appeared 15 February in Molecular Psychiatry.
The results hint that only some TSC mutations boost protein synthesis. “That’s the beauty of science: Nothing is so clean,” says Tsai, who was not involved in the study.
Researchers can use these neurons to screen drugs for tuberous sclerosis.
“Not only can we test the things that we know work in the mouse models, like rapamycin, but we can look for additional therapeutic targets,” says lead researcher Mustafa Sahin, professor of neurology at Harvard University.
By joining the discussion, you agree to our privacy policy.