THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.
The gene SHANK3, a leading candidate for autism risk, helps sensory neurons respond to pain, according to a study in mice. The findings may provide a genetic explanation for the high pain threshold seen in some people with autism.
SHANK3 is mutated in about 2 percent of people with autism. It is missing in people with Phelan-McDermid syndrome, a condition marked by autism, severe intellectual disability and a blunted sensitivity to pain. Individuals with either condition often show a muted response to extreme temperatures or pressure.
Most studies of SHANK3 have focused on the gene’s role in the central nervous system, where it supports communication between neurons. The new study, published 1 December in Neuron, reveals a role for SHANK3 in sensory neurons just outside the spinal cord. This makes SHANK3 necessary for the proper perception of pain.
“We made a surprise finding that SHANK3 is expressed in the peripheral nervous system,” says lead investigator Ru-Rong Ji, professor of anesthesiology at Duke University in Durham, North Carolina.
Ji and his colleagues studied mice missing one or both copies of SHANK3. These mice have features reminiscent of autism, such as impaired neuron signaling, social problems and repetitive behaviors.
The mice respond normally to certain painful stimuli, such as hot and cold temperatures and puncture wounds, the new study found. But mice with a foot that is already inflamed from bacterial infection do not perceive as much pain from heat as controls do.
Peripheral issue:
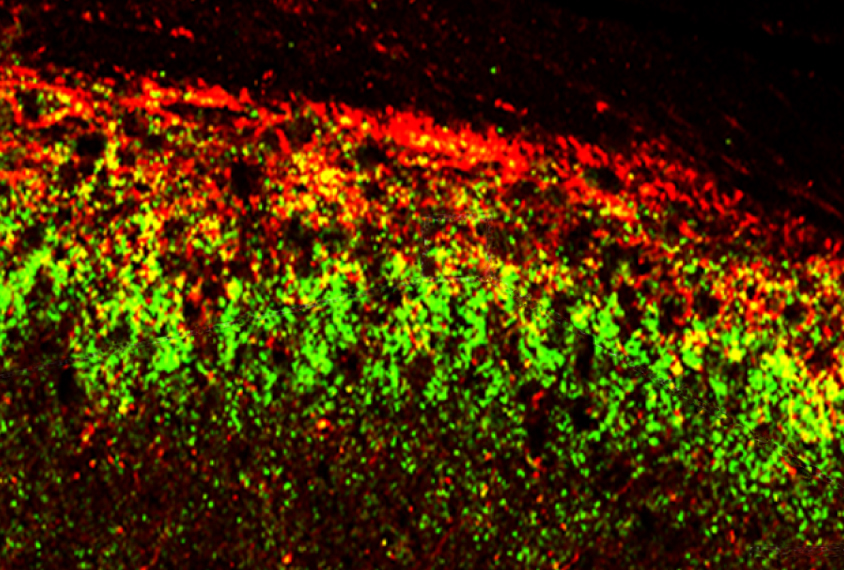
The neurons that sense inflammatory pain reside in the dorsal root ganglion, a bundle of nerves that nestles against the spinal cord and relays sensory information from the rest of the body. Ji and his team examined cells from the dorsal root ganglion of SHANK3 mice.
In control mice, SHANK3 tethers a protein called TRPV1 to the surface of sensory neurons, where it detects heat and chemical signals. Those signals activate TRPV1, causing calcium ions to flood into the cell, leading to a painful sensation.
Neurons from control mice show a robust influx of calcium ions in response to capsaicin, the chemical that gives chili peppers their heat. But the chemical triggers significantly less calcium flow into neurons from SHANK3 mice.
Ji and his team engineered a third strain of mice, lacking SHANK3 only in the sensory neurons of the dorsal root ganglia. These mice show a decrease in sensitivity to inflammatory pain similar to that seen in mice missing SHANK3 everywhere. The finding also suggests that the insensitivity to pain seen in SHANK3 mice stems from sensory neurons and not from the brain’s inability to process pain signals.
The study stokes curiosity about the connection between autism and TRPV1. This protein aids heart and lung function, and has been linked to addiction, anxiety and depression, says Camilla Bellone, assistant professor of neuroscience at the University of Geneva in Switzerland, who was not involved in the study. “It would be really interesting to see if TRPV1 dysfunction could explain other [features] associated with autism,” she says.
By joining the discussion, you agree to our privacy policy.