Most people with fragile X syndrome express the gene FMR1, which is mutated in the syndrome, a new study shows.
The findings are at odds with the prevailing theory that fragile X mutations silence FMR1, says lead investigator Joel Richter, professor of molecular medicine at UMass Chan Medical School in Worcester, Massachusetts. “It was a shocking and astonishing result, at least to me,” he says.
Instead, the mutations promote the expression of an alternate RNA version of the gene over its full-length counterpart — an issue that can be corrected, at least in blood cells, using antisense oligonucleotides, the study shows.
Fragile X syndrome is characterized by intellectual disability, seizures and — in one in three cases — autism. A fragile X mutation consists of more than 200 repeats of the DNA letters “CGG,” which cause methyl groups to cluster on the gene and, purportedly, block FMR1 gene expression. Loss of FMRP, the protein that FMR1 encodes and a key modulator of neuronal connections, leads to fragile X syndrome.
“A lot of models are based on FMR1 being absent,” says Eric Klann, professor of neural science at New York University, who was not involved in the study. “It’s important to know that a subset of patients express FMR1, [as] it could be targeted therapeutically,” he adds.
W
To see whether splicing issues occur in people with fragile X syndrome, Richter and his colleagues sequenced RNA from the white blood cells of 29 men with fragile X syndrome and 13 men without the condition.
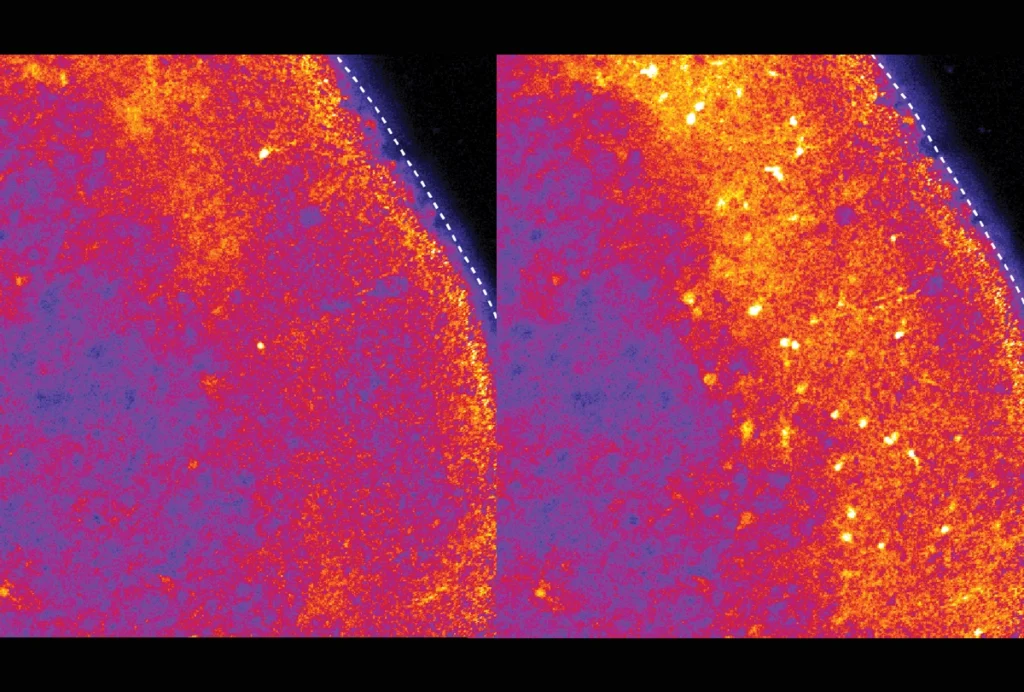
By sequencing sections of RNA and mapping the short reads to various isoforms, the researchers found that about 10 percent of genes expressed in fragile X cells are atypically spliced. This includes the supposedly silent FMR1 gene, which was expressed by cells from 21 of the men with fragile X, 4 of whom had expression levels that were similar to or exceeded those of controls. They express an RNA version of the gene that is shorter than usual, and potentially nonfunctional. By contrast, the men without fragile X express a version that contains all of the gene’s coding regions.
The researchers also detected the stunted isoform in postmortem brain slices from three out of six people with the condition. And it turned up in publicly available RNA sequencing data from “premutation” carriers — who harbor 55 to 200 CGG repeats, which is long enough to dampen FMRP but not enough to cause the full-blown syndrome. This result suggests that defective splicing may be implicated in conditions associated with the premutation, such as motor or fertility problems.
Analysis of skin samples from three additional premutation carriers confirmed the presence of the misspliced isoform in one of them. This person harbored 140 repeats, whereas the other two premutation carriers had fewer than 100. The results hint that the repeat sequences drive the defective splicing, Richter and his colleagues say.
A
To boost FMRP, the researchers created a panel of antisense oligonucleotides (ASOs) — short snippets of RNA that can modify splicing — designed to bind FMR1. When they tested the ASOs on blood cells expressing the misspliced RNA, a combination of two turned down production of the truncated transcript and amplified the full-length version. FMRP levels also increased, the researchers found.
But the strategy would be ineffective for the subset of people with fragile X who don’t express FMR1. In cells from these people, the team tested the ASOs alongside a methylation inhibitor, a compound previously shown to activate FMR1. The combined treatment successfully increased levels of the full-length transcript and its encoded protein more than the inhibitor alone.
So far, demethylation-based approaches have met with limited success, possibly because of defective FMR1 splicing, Richter and his colleagues say. Treatments that combine DNA demethylation with ASOs might be a useful strategy for those with a fully silenced FMR1 gene, they say.
The results were published online on 26 June in the Proceedings of the National Academy of Sciences.
T
So far, “therapeutic approaches have largely centered on reversing transcriptional silencing,” says Antonio Bedalov, professor of medicine at Fred Hutchinson Cancer Research Center in Seattle, Washington, who was not involved in the study. But this approach may need to be combined with ASOs to be effective, he says.
ASOs are already being used to treat spinal muscular atrophy, and clinical trials are underway for Angelman syndrome, a rare genetic condition linked to autism. Now, “we just need to figure out the best way of applying it to fragile X individuals,” he says.
But others think the focus on treatments may be premature.
Detection of the isoform using long-read technologies — a more accurate method of sequencing repetitive DNA — is “critically needed,” says Lilia Iakoucheva, professor of psychiatry at the University of California, San Diego, who was not involved in the work.
And only half of the brain samples expressed the misspliced isoform, Iakoucheva says. Identifying the isoform in cultured neurons, which have different transcriptional profiles than blood cells do, is an important next step, she adds.
Indeed, repeating their findings in brain organoids and neurons derived from people with fragile X is Richter’s next move. His team also hopes to uncover how the heavily methylated gene is expressed, and how mutations skew splicing. “Our list of things to do is pretty long,” Richter said in a video interview with Spectrum last month, glancing up at the to-do list scrawled on his office blackboard.