Immune molecule alters cellular makeup of human brain organoids
The changes may help explain the link between maternal infection and autism, though more research is needed.
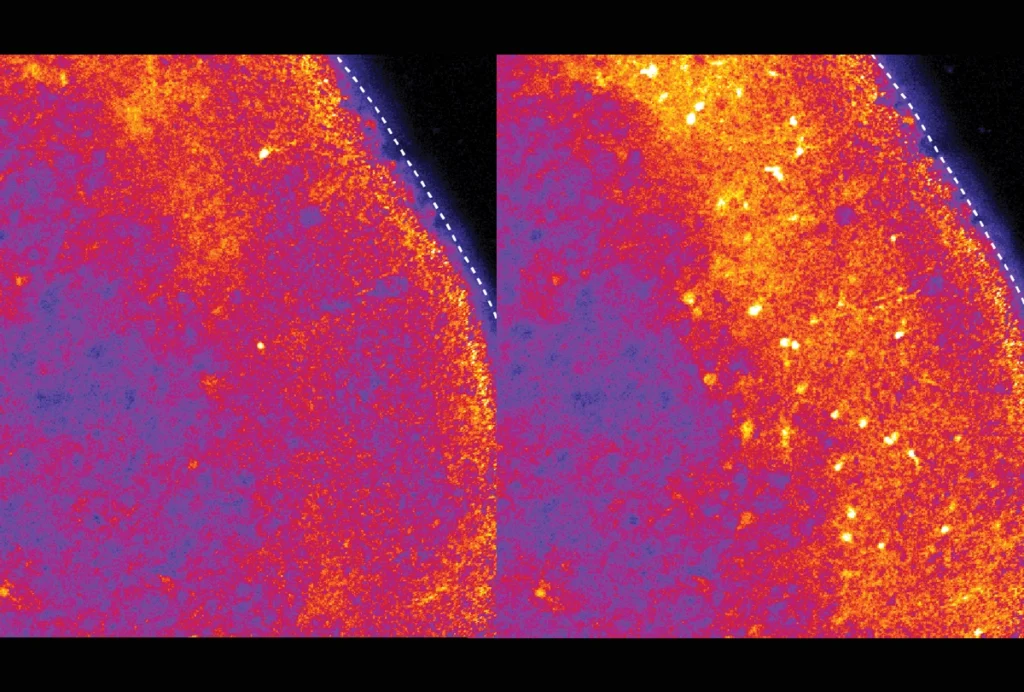
Human brain organoids exposed to an immune molecule show an increase in radial glia cells — key precursors to many brain cells — as well as changes in gene expression, a new study finds.
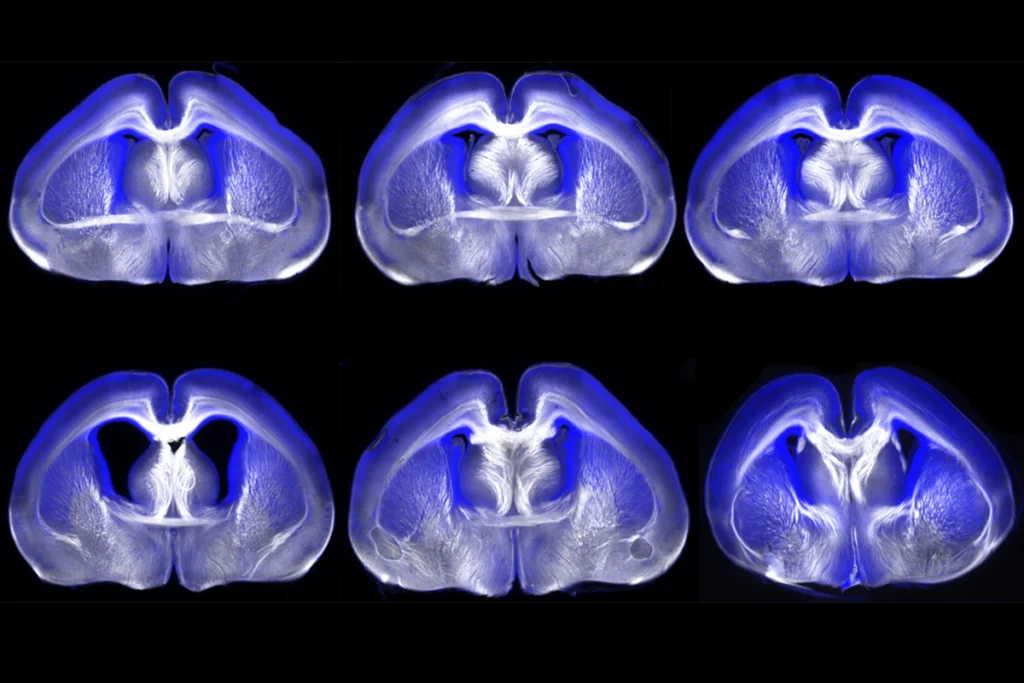
The results jibe with those from mice exposed prenatally to the molecule. Further experiments on these brain organoids may help scientists understand why severe infection during pregnancy is linked to a slightly increased chance of having an autistic child.
“For the first time, we have shown that brain organoids can be used to model the effects of maternal immune activation on brain development and that our results are generally coherent with mouse models,” says lead investigator Simone Mayer, an independent research group leader at the Hertie Institute for Clinical Brain Research at the University of Tübingen in Germany.
Interleukin-6 (IL-6), a molecule secreted by white blood cells in response to infection, can trigger inflammation and influence fetal brain development in mice, previous studies suggest.
To see if those findings translate to people, Mayer and her colleagues grew brain organoids from human stem cells and treated them with hyper-IL-6, a highly potent version of IL-6. To mirror the way IL-6 spikes in the body after an infection, Mayer’s team treated the organoids for 5 to 10 days, starting on day 45 of their growth when they mimic the neocortex during early mid-gestation. The neocortex is the most recently evolved part of the brain and is key to sensory perception, conscious thought and language.
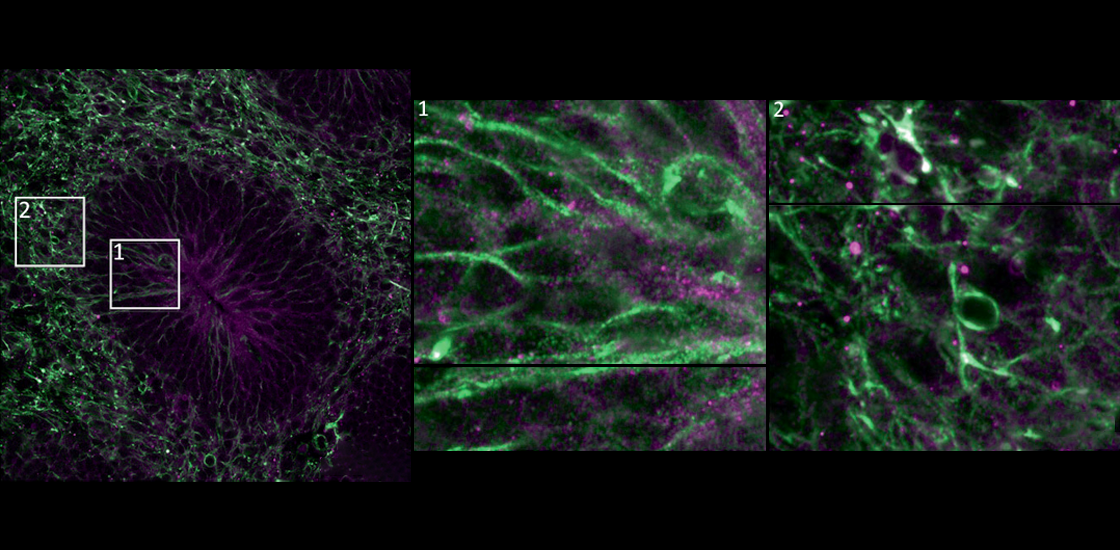
The treatment slightly boosted the organoids’ levels of radial glia cells, which give rise to neurons and have protrusions that “serve like railways for young neurons to migrate to their final location,” Mayer says, and so “support the correct layering of the neocortex.”
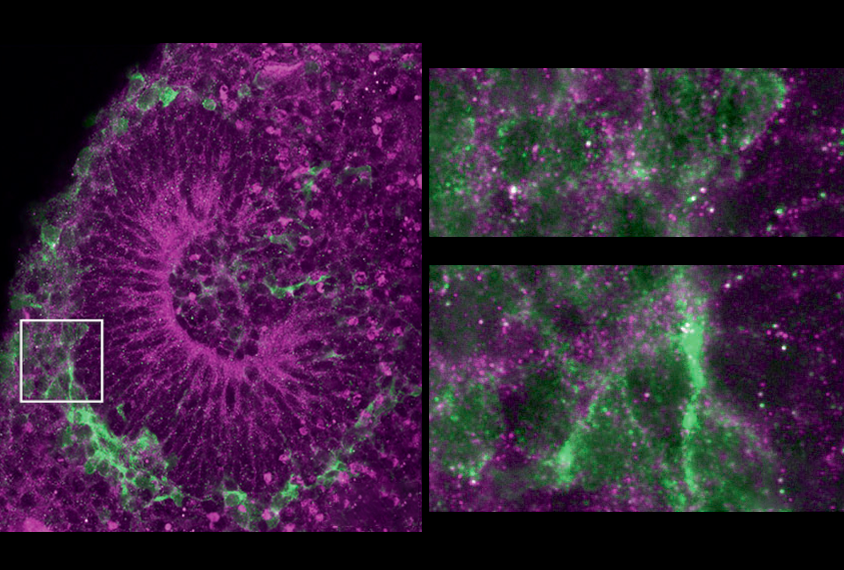
This result may explain why the organoids later show abnormal changes in the number and position of upper-layer neurons 35 days after hyper-IL-6 treatment.
This work “adds to the growing literature that suggests autism spectrum disorder is related to abnormal neuroprogenitor differentiation leading to alterations in the proportion of cell types in the brain,” says Brady Maher, lead investigator at the Lieber Institute for Brain Development in Baltimore, Maryland, who was not involved with the study.
O
The scientists also identified genes whose expression changed after immune reactions in the organoids but not in previous mouse models of maternal immune activation. Although animal models are useful in analyzing aspects of autism and other neurodevelopmental conditions, “they may not fully reflect the complexity of the human brain and its development,” Mayer says.
The scientists detailed their findings on 6 March in Molecular Psychiatry.
The study’s main drawback is the organoids’ lack of immune cells called microglia, which mediate responses to maternal immune activation, Mayer says. She and her colleagues plan to incorporate microglia in future studies.
In addition, the organoids were derived from the stem cells of neurotypical men. Future research should test organoids grown from autistic people “with and without a history of maternal infection during their fetal development,” Maher says. “This may allow us to tease out how the individual’s genetics responds to environmental insults.”
Future studies should also generate organoids from female cells and test other immune molecules, such as IL-17A, says Rose Glass, a doctoral candidate in Jason Stein’s lab at the University of North Carolina at Chapel Hill, who was not involved with the study.
Mayer agrees, noting that “in mouse models of maternal immune activation, male offspring responded with more severe dysregulation. Considering that the prevalence of autism diagnosis is higher in boys compared to girls, the question is whether girls have resilience mechanisms.”
All in all, the findings “affirm a longstanding concern about the potential effects of maternal infection during pregnancy on fetal development,” says Christopher Coe, professor emeritus of biopsychology at the University of Wisconsin-Madison, who was not involved with the study. However, “as exciting as ex-vivo cellular models are, one still needs to confirm the findings with in-vivo studies.”
Explore more from The Transmitter
RNA drug corrects calcium signaling in chimeric model of Timothy syndrome