Microscopic electronic probes implanted within blood vessels in rats can record single-neuron activity without brain surgery, a new study finds.
The new devices may one day enable long-term minimally invasive recording deep within the brain.
“We could envision providing a quantum jump forward that may help to better understand the underlying brain factors important in autism,” says study investigator Anqi Zhang, a postdoctoral fellow in chemical engineering and bioengineering at Stanford University in California. Zhang says the technique could also help study the effects of medication on the brain.
Brain-monitoring devices typically involve trade-offs between how invasive and how sensitive they are. For instance, electroencephalography is noninvasive but cannot target individual neurons. It is limited to scanning neural activity at the brain’s surface. By contrast, recording single-neuron activity from deep within the brain often requires an invasive procedure to implant probes. Infection, inflammation and damage to brain tissues can result.
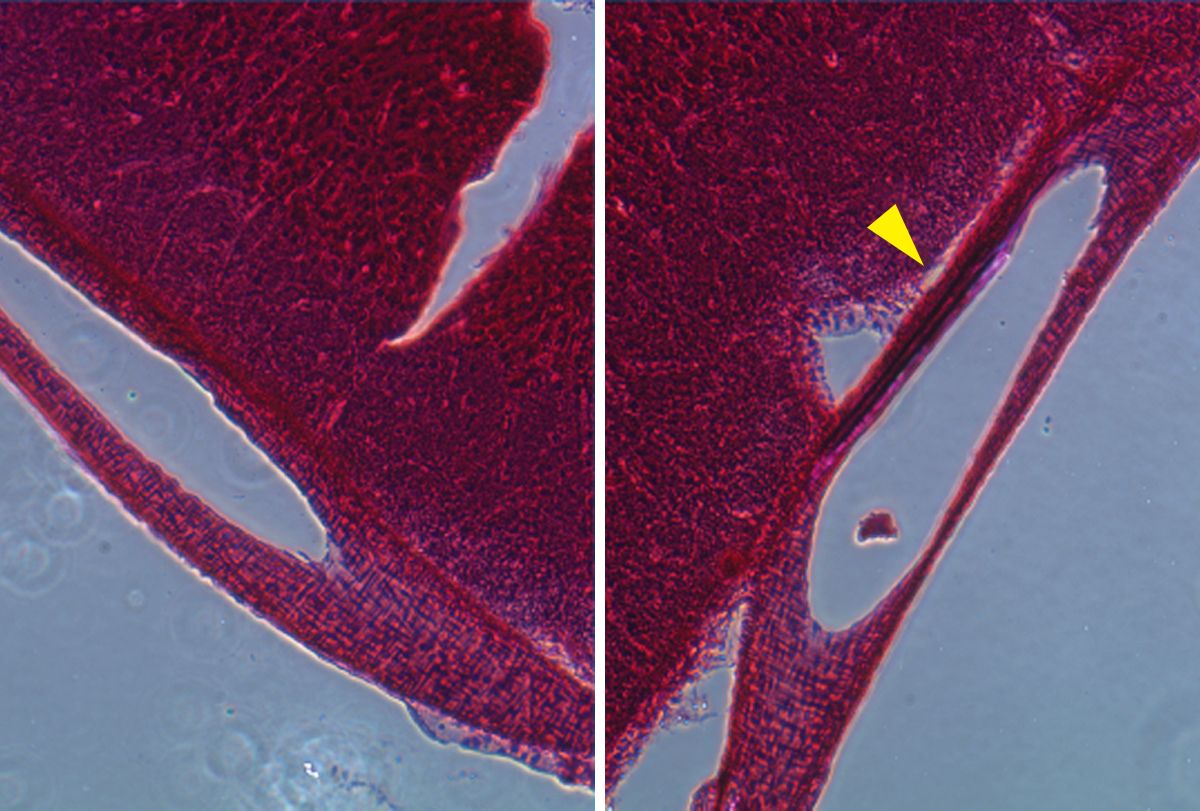
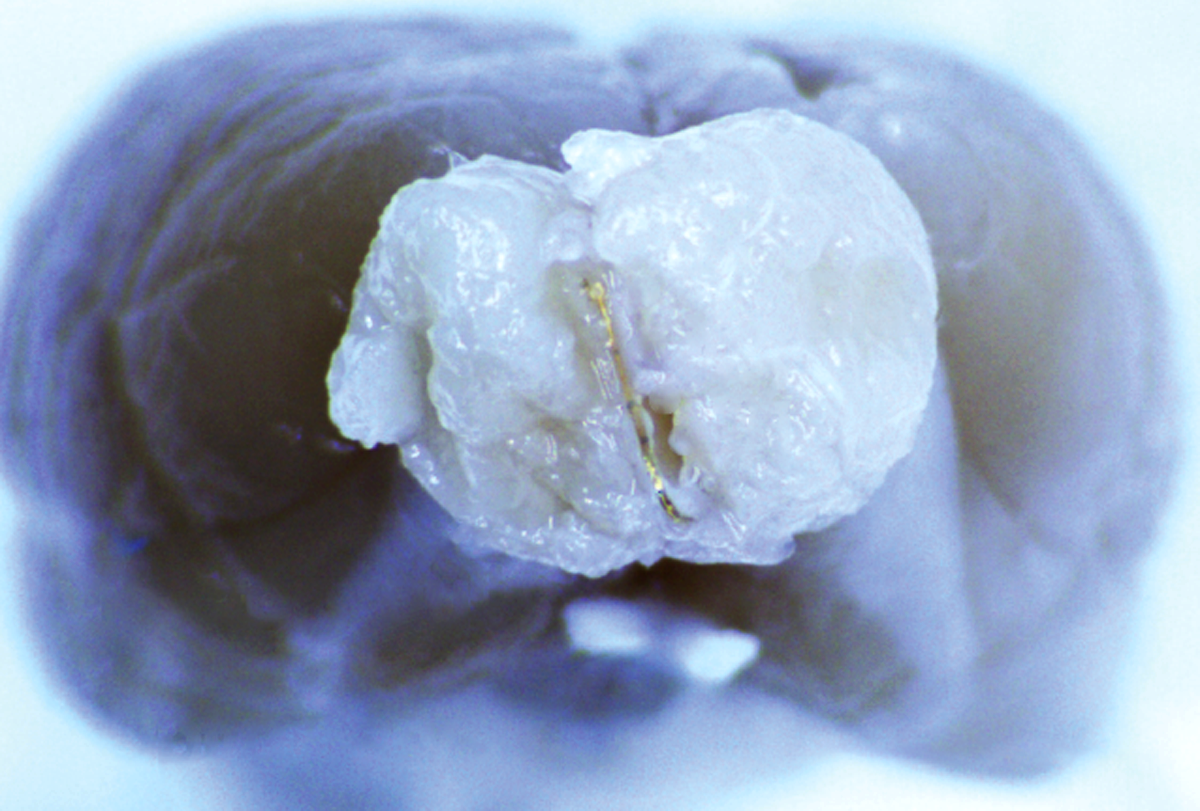
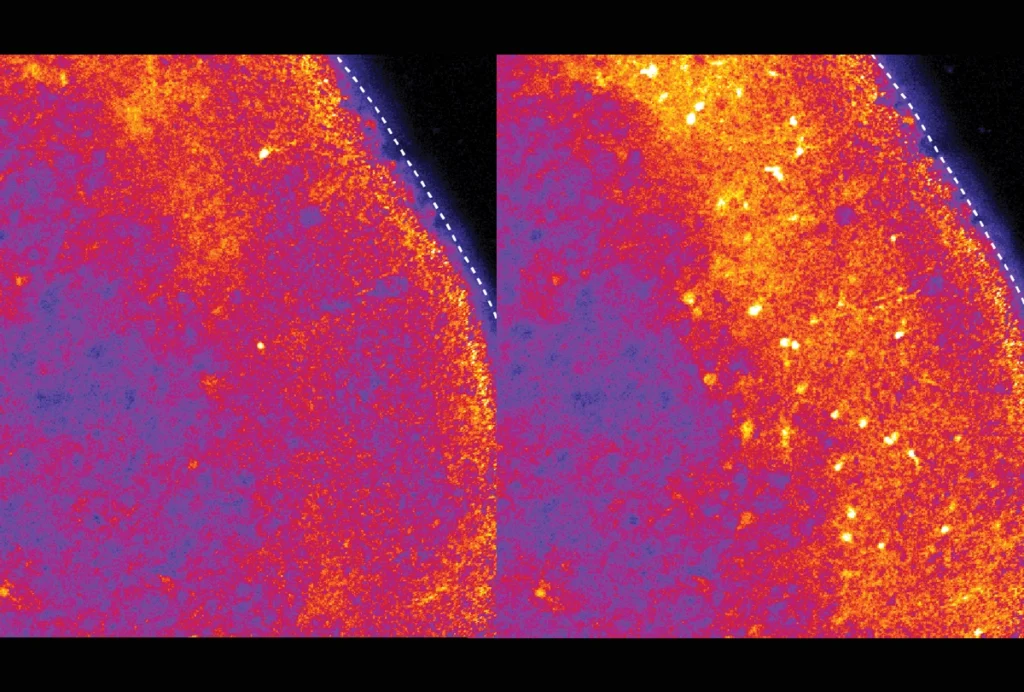
But with this new approach, Zhang and her colleagues demonstrated that they could record activity from the cortex and olfactory bulb through blood vessel walls down to the single-neuron level. The technique was less invasive than brain surgery, and the team detected no negative consequences to rodents’ health. Using this approach, they could pinpoint and monitor seizure activity induced by penicillin injections. (Epileptic seizures may occur in nearly half of individuals with autism.)
Though the probes have yet to be tested in people, “Accessing the brain via the vessels, as opposed to the skull, is likely a much more agreeable procedure to patients,” says György Buzsáki, professor of neuroscience at New York University, who did not take part in this research. He praised the work, noting that “the high-quality recordings are excellent, and the approach has promise.”