THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.
Mutations in a set of neurons that dampen brain activity may be the source of seizures in an autism-related condition. The neurons lack UBE3A, the gene mutated or missing in Angelman syndrome and duplicated in some cases of autism.
The findings, published 6 April in Neuron, call out this subset of inhibitory neurons as a key player in Angelman syndrome1.
About 90 percent of children with Angelman syndrome have seizures, and many of them do not respond to epilepsy drugs, says lead researcher Benjamin Philpot, professor of neuroscience at the University of North Carolina at Chapel Hill. “If we can home in on how UBE3A loss is altering circuitry, I think that will give us more clues as to what therapeutics will help.”
In 2012, Philpot and his colleagues reported that mice lacking UBE3A in all neurons have diminished inhibitory activity in one small circuit in the brain2. Later that year, another team showed that boosting inhibition with an experimental sleep drug eases the motor coordination problems seen in a mouse model of Angelman syndrome.
The findings hinted at a shift in the balance between excitation and inhibition in the brain in Angelman syndrome, but whether this shift was solely the result of too little inhibition was unclear. The researchers couldn’t rule out whether too much excitation was also involved. “There are many ways you can get off the main road,” Philpot says.
Understanding the precise scenario would allow researchers to develop more targeted drugs for seizures, says Lawrence Reiter, associate professor of neurology at the University of Tennessee Health Science Center, who was not involved with the work. This is “a huge step forward in terms of seizure treatments for Angelman syndrome,” he says.
Recycling snag:
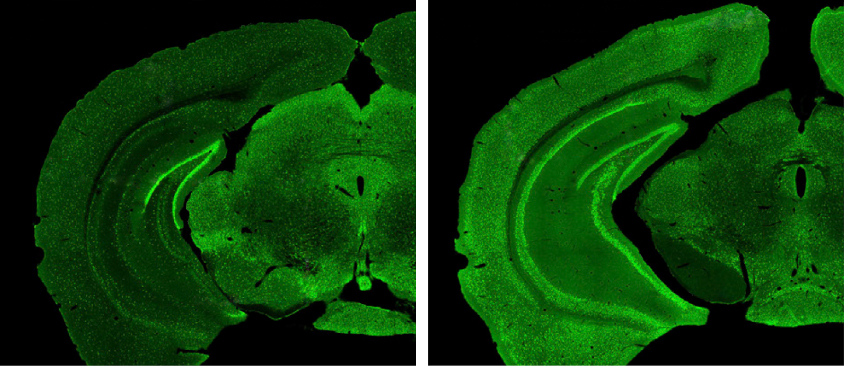
Philpot and his team deleted UBE3A in either of two sets of mouse neurons: those that excite brain activity and those that inhibit it. The mice missing the gene in inhibitory neurons have spontaneous seizures and are unusually susceptible to seizures when exposed to a convulsant drug or loud noise.
Those lacking the gene in excitatory neurons, by contrast, do not have spontaneous seizures and are no more susceptible to seizures than are controls, suggesting that defects in inhibitory neurons — not excitatory ones — underlie the seizure activity in Angelman syndrome.
The mice with altered inhibitory neurons also show abnormalities in brain activity, detected by electroencephalography — which picks up synchronous electrical patterns from groups of neurons.
These mice have more severe seizures than those that lack the gene in all of their neurons, and roughly 15 percent of them die before reaching 3 months of age. Virtually all of the mice with UBE3A deleted in all of their neurons lived at least 3 months. The researchers say a global lack of UBE3A may also depress excitation, thereby balancing out the abnormal inhibition.
In their 2012 study, Philpot and his team showed that deleting UBE3A wholesale prevents the recycling of the chemical-filled bubbles, or vesicles, that neurons release upon firing. The new study shows that mutated inhibitory neurons contribute to this recycling defect, providing a more precise target for seizure treatment.
The study also suggests that other neurons contribute to a signaling imbalance in Angelman mouse brains.
Overall, the findings highlight how little is known about UBE3A’s effects on the brain, says Scott Dindot, associate professor of molecular medicine at Texas A&M University in College Station, who was not involved in the new study. “We’re learning a lot about UBE3A and there’s a lot to learn,” Dindot says. “These fine-tuned studies are what it’s taking to really figure this out.”
By joining the discussion, you agree to our privacy policy.