THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.
MeCP2, a gene associated with neurodevelopmental conditions such as Rett syndrome and autism, has an unexpectedly essential role in mature brains, a new mouse study suggests. The findings support the idea that delivering treatment in adulthood can treat symptoms of the condition.
Rett syndrome emerges in early childhood, leading to seizures, motor problems and intellectual disability, among other symptoms. (In boys, who have only one copy of MeCP2, the disorder is fatal.) But the new study shows that losing MeCP2 has the most dramatic effect after the brain reaches maturity1.
“When the mice reach adulthood, the brain completely cannot function without MeCP2, not even for a few days,” says lead researcher Nurit Ballas, research professor of biochemistry and cell biology at Stony Brook University in New York.
The work adds to growing evidence that MeCP2 has an important a function in adulthood: A 2012 paper showed that blocking the MeCP2 protein’s production in the mature brain leads to Rett-like symptoms in mice. And researchers have reported that restoring its function in adult mice can ease many of these symptoms, indicating that MeCP2 plays a maintenance role in the brain.
The new findings, published 16 February in Human and Molecular Genetics, highlight the transition to adulthood as a critical period for MeCP2 function.
The study suggests that shutting down MeCP2 in a mature brain makes the brain revert to a more immature state: It shrinks and neurons lose their sophisticated features. It is as if the brain comes to rely on the protein more and more as it matures, says Huda Zoghbi, professor of molecular and human genetics at Baylor College of Medicine in Houston, Texas.
“The more we depend on this protein, the more we’re vulnerable and acutely sensitive to its loss,” says Zoghbi, who was not involved in the study. “That’s really the big conclusion here.”
Sudden onset:
To examine the effects of lack of MeCP2, Ballas and her colleagues engineered male mice in which the researchers could shut down production of the MeCP2 protein at any time by injecting a drug called tamoxifen. They injected the drug in mice of various ages and then rated the severity of mobility problems, tremors, repetitive behaviors and other Rett-like features in the mice.
Shutting down MeCP2 in 15-week-old mice — the mouse equivalent of adulthood — sparks an immediate decline. These mice show severe Rett-like symptoms within a few days. Half of the mice in the study die within a week and none survive past three weeks. The same sudden onset occurs when mice lose MeCP2 later, at 30, 34 or 48 weeks.
By contrast, shutting off the gene in 10-week-old mice, the mouse equivalent of adolescence, leads to a much slower emergence of features. Roughly a month after the gene is turned off, the mice have only mild symptoms and survive for months.
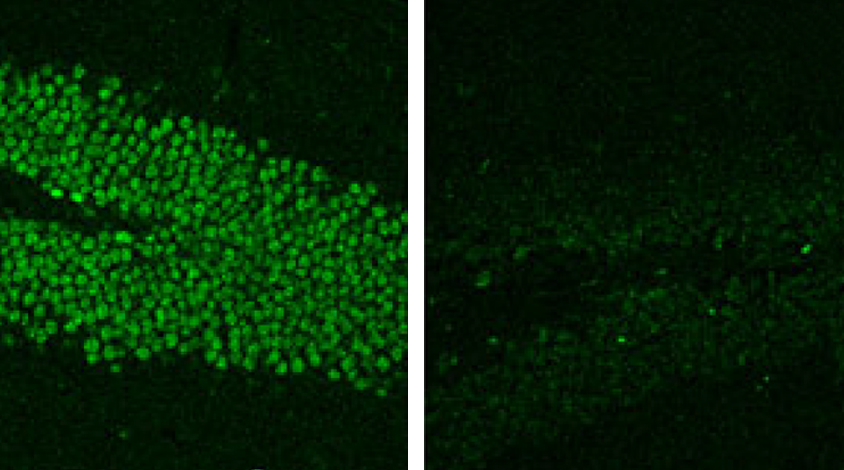
The researchers found a similar pattern in the mouse brains, in which later loss of the protein produces more pronounced changes. Losing MeCP2 at 15 weeks or later leads to an immediate decrease in brain size. It also spurs a rapid decrease in the number of signal-receiving branches on neurons, called dendritic spines, and the spines also shorten.
“It’s really dramatic, as if the brain has no way to quickly compensate,” says Ype Elgersma, professor of molecular neuroscience at Erasmus Medical Center in Rotterdam, the Netherlands, who was not involved in the study. “I couldn’t believe it when I saw it.”
Protein pawns:
Shutting off MeCP2 at 10 weeks, however, does not instantly diminish the number of dendritic spines in the brain. After a month, just about a quarter of the spines are truncated, and only months later do they decline in number.
Removing MeCP2 in adulthood may have particularly powerful effects, because the mature brain is less adaptable than it is in youth, and can no longer compensate for the loss. “I think that this means that in the adult brain, there is really no plasticity anymore around MeCP2 pathways,” Elgersma says.
To assess the significance of the timing, Ballas and her colleagues tracked changes in the brains of typical mice between 10 and 15 weeks. They saw the brain grow and its spines mature — until 15 weeks, when both processes plateau, suggesting that the brain reaches maturity at that point, says Ballas.
The researchers then looked at how loss of MeCP2 affects proteins that function at synapses, the junctions between neurons. Shutting down MeCP2 expression at 15 weeks cuts the levels of some of these proteins, but not others. In typical mice, expression of the affected proteins surges between 10 and 15 weeks.
“I thought it was very interesting that certain pathways are really changed by loss of MeCP2, and others are not at all affected,” Elgersma says. “That should lead to insight into the molecular mechanisms that MeCP2 controls.”
By joining the discussion, you agree to our privacy policy.