THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.
A new method allows scientists to chemically coax immune cells in blood into becoming mature neurons. Generating neurons from people with autism with the technique, described 8 March in Stem Cell Reports, could help researchers understand how autism-related mutations affect the brain, and help them screen medications for the condition1.
Scientists typically convert blood or skin cells into neurons by first reverting them back into stem cells, which can become any cell in the body. Then they bathe the induced stem cells in a chemical soup that turns on the expression of genes needed for them to become neurons.
But using skin cells requires removing small pieces of skin, which can be painful and lead to infection and scarring. Drawing blood is less invasive, but blood contains a mixture of different cell types, which may produce a nonuniform population of neurons.
Starting with blood-borne, infection-fighting cells called T cells sidesteps these problems. The researchers isolated skin cells and T cells from a man with no neurological conditions and converted both sets into stem cells. They then found that four established methods for converting stem cells into neurons work for the skin-derived stem cells but not for the T-cell-derived ones.
Starving cells:
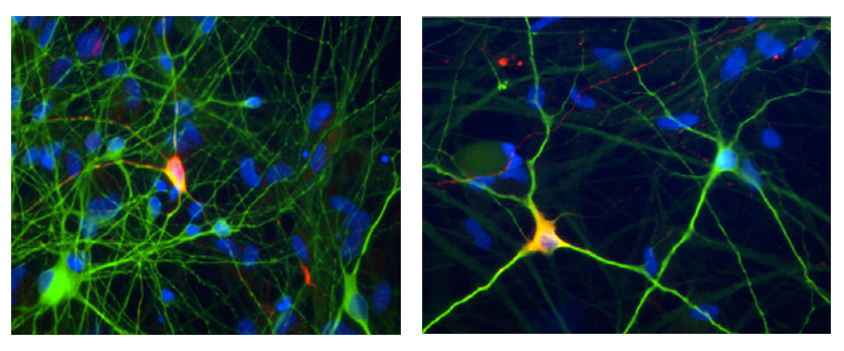
The researchers then tried suspending the stem cells in a chemical broth containing little oxygen and low levels of nutrients. These conditions are known to cause stem cells to express molecules that are markers for neurons and to protect them from death. In this broth, stem cells derived from both skin cells and T cells efficiently morph into neural precursors, particularly precursors from areas of the developing brain believed to be important in autism.
After 60 days in culture, both sets of neural precursors develop into a mixture of mature neurons that communicate using the chemical messengers dopamine, glutamate or gamma-aminobutyric acid. Neurons derived from the T cells show signaling properties similar to those that arise from skin cells, suggesting that both sets are mature and functional.
When the researchers used the new method with T cells of a man with Parkinson’s disease, they found that the resulting neurons that communicate using dopamine — the type depleted in the condition — are particularly vulnerable to cell death. The neurons also showed other signs of Parkinson’s disease, such as damaged mitochondria and high levels of chemically reactive molecules.
Using T cells to derive neurons could help scientists gain a better understanding of Parkinson’s disease and, perhaps, autism.
By joining the discussion, you agree to our privacy policy.