Taking acetaminophen during pregnancy is not associated with an increased chance of having a child with autism, attention-deficit/hyperactivity disorder (ADHD) or intellectual disability, according to a study published today in the Journal of the American Medical Association.
Any previously reported associations are “likely due to familial confounding,” says Brian Lee, associate professor of epidemiology at Drexel University and lead investigator of the work. “It’s not a causal effect.”
The findings come just months after a U.S. federal judge found insufficient scientific support for claims that prenatal exposure to acetaminophen, marketed as Tylenol, causes autism and ADHD, as a class-action lawsuit against its manufacturers and retailers had alleged. As a result, the judge blocked expert witnesses from testifying; the plaintiffs plan to refile their lawsuits in state courts, according to one of the law firms involved.
Prior studies had found a correlation between acetaminophen use and neurodevelopmental conditions, which led to a 2021 consensus statement from doctors and scientists that called for additional research and warned against taking the drug during pregnancy if not needed. But those previous studies did not capture the full picture, Lee says, because they did not adequately control for confounding factors.
Some of those unchecked confounding factors include parental health and genetics, says Gretchen Bandoli, associate professor of pediatrics at the University of California, San Diego, who was not involved in the work. It’s also difficult to study acetaminophen exposure because it is an over-the-counter drug and has a short half-life in the body, she adds. And the reasons for taking acetaminophen—fever, pain or infection—may themselves increase the likelihood of having a child with a neurodevelopmental condition.
“You can repeat the same biased thing over and over again, and you’ll keep getting the same biased association,” Bandoli says of the previous analyses.
T
he new study compared children who were exposed to acetaminophen in utero with their siblings who were not. “Siblings share genetics; they share the environment,” Lee says. “So you can control for a lot of unknowns that you may not be able to measure.”The ideal approach would be a randomized clinical trial, but this is not possible given the range of medical reasons for taking acetaminophen, Lee says. “The people who take a drug are going to be very different from the people who don’t take the drug. Because we can’t possibly begin to capture all of the reasons behind why someone may or may not take acetaminophen, we can’t necessarily adjust for those in our statistical models.”
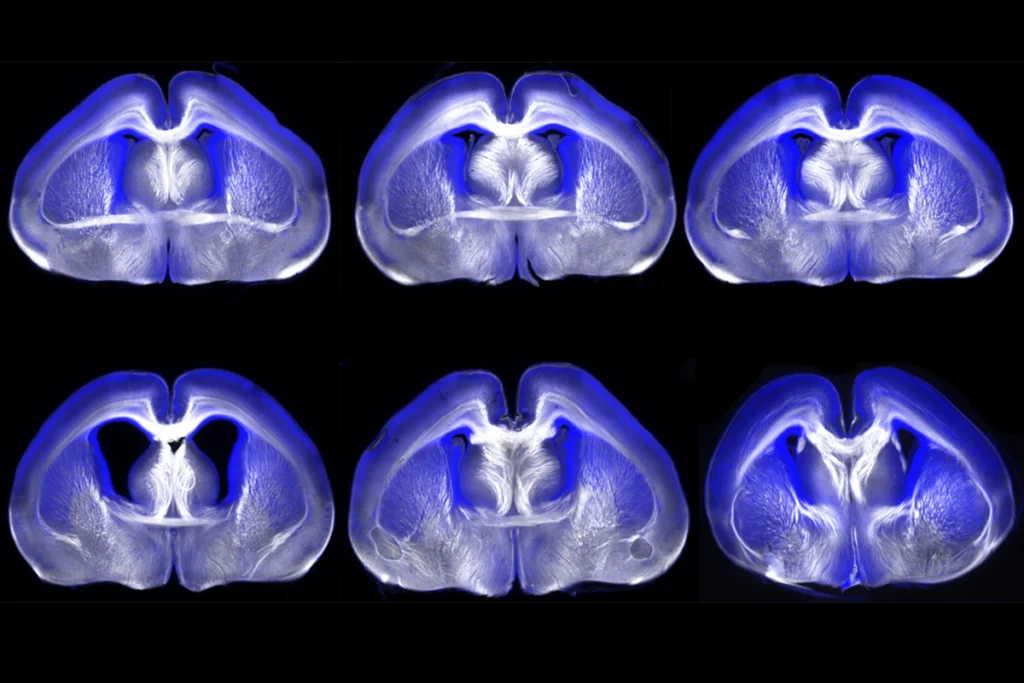
Lee’s team examined several population and health registries in Sweden for all people born between 1995 and 2019 and pulled out sibling sets with at least one acetaminophen exposure—a cohort of more than 1.7 million children in total. Sweden’s birth register contains information about the chronic use of medications, including acetaminophen, collected by midwives during structured interviews with women starting when they are 8 to 10 weeks pregnant and throughout the course of the pregnancy. The researchers supplemented this information with acetaminophen prescription dispensations from the country’s prescription drug register.
Children exposed to acetaminophen during gestation “were slightly more likely” to be diagnosed with autism, ADHD or intellectual disability than children who were not exposed, Lee and his colleagues write in the study, but the association vanished when he compared siblings with each other.
“This is, by some distance, the best study out there,” says Per Damkier, professor of clinical pharmacology at the University of Southern Denmark, who was not involved in the work. “The overall design of the study—the analytical approach—is very, very meticulous.”
T
he sibling design controls for the myriad factors that go unchecked in a traditional design, Bandoli says. In addition to parental health and genetics, it also accounts for income level and education, assuming those factors remain constant for children born to the same parents.One limitation to the sibling design is that it assumes the parent’s behavior did not change between pregnancies, Damkier says. “And that may not be entirely true, but still, it’s the best you could do.”
In the new work, parent behavior did change in at least one critical way, Bandoli says: The parent took acetaminophen during one pregnancy but not another. “There tends to be a medical reason why they change their behavior,” Bandoli says, such as the pregnant parent contracting a virus.
Another limitation is that the sibling design may amplify biases and mask the effect of mediating variables, or those that help explain why an exposure contributes to the increased chance of a disease or condition, say Ann Bauer, research epidemiologist at the University of Massachusetts Lowell, and Shanna Swan, professor of environmental medicine and public health at the Icahn School of Medicine at Mount Sinai, in a written statement shared with The Transmitter. Bauer and Swan were involved in the 2021 consensus statement but not the new study.
Biases can indeed become more pronounced in sibling comparisons, Lee and his colleagues say in a written response shared with The Transmitter. But the slight difference in autism likelihood observed in the full cohort is so minor that it could easily be caused by unmeasured cofounders, Lee and his team say, since the study is “observational by nature.”
A
bout 7.5 percent of children in the analysis were exposed to acetaminophen in utero, the study found. “That’s a lot lower than we would have seen in a U.S. study,” Bandoli says. The finding fits within the range reported in other studies, Damkier says, which span from about 6 to 60 percent, but is relatively low and could therefore limit the generalizability of the results to countries other than Sweden.The low percentage could also be a sign of missed exposures and “bias results toward the null,” Bauer and Swan say in their written statement. If that were the case, Lee’s team points out in its written response, it would not explain why their crude analysis mirrors the results of previous studies. “It’s not like our study was biased toward finding nothing,” Lee says. “We started out at exactly the same level.”
Plus, prior studies defined exposure in different ways, including one-time use of the drug, says Nathaniel DeNicola, an OB-GYN and chief medical officer of Caduceus Medical Group, who wasn’t involved in the study. The design of Lee’s study is stronger because it relies on midwife-led interviews during pregnancy, rather than giving participants surveys months or years later, as in other studies, he says. And none of the studies—including Lee’s—include exact dosages of the medication, DeNicola says.
An exposure rate of about 7 percent aligns with what DeNicola encounters as a clinician, he says. “Widespread use of Tylenol during pregnancy is simply not an issue.”
DeNicola says he hopes this study quells the concerns of expecting parents, so they feel more comfortable taking acetaminophen when it is medically required. “Having an untreated fever during pregnancy statistically is worse than taking this medication for those rare occasions.”